Introduction
Nurses worldwide are increasingly working in environments characterized by healthcare reforms, complex patient care and technological advancements that require the integration of evidence-based practice (1,2). These changes require nurses who are competent in leadership, health policy, system improvement, research, evidence-based nursing (EBN) and collaboration—all of which are essential in facilitating the delivery of high-quality care (3-10). Having qualified faculty to educate advanced practice nurses (APNs) to meet these new challenges is crucial. Indeed, there is an ongoing trend of advancement in nursing education, such as pursuing master’s degrees in nursing specialties (3,9,11,12).
There is also a growing need for continuous education, systematic competence research and competence assessment instruments to meet the rapid changes in critical care settings (13). Continuing professional development within advanced nursing acts as a source of inspiration and motivation towards the achievements of goals and objectives within advanced nursing (10,14). It also emphasizes professional and interprofessional learning opportunities in the clinical field. Continuing professional development and master’s degrees in nursing may ultimately affect patient care (6,15).
History and context
NAs and ICNs are expected to deliver holistic, evidence-based, person-centred care to patients with life-threatening conditions, as well as to the patients’ families (1,16). For optimal patient care, advanced nursing competences must be aligned with the patients’ needs, available technology, illness severity and level of patient dependency (17,18).
Nurses’ engagement in continuing professional development varies across European countries and other parts of the world, and it can be either mandatory or voluntary (19,20). In Norway, it is voluntary, though a recent Norwegian study has highlighted research-based master’s theses as important contributors to knowledge building in nursing (5). And despite the authors’ assertion that systematic knowledge building is crucial in a rapidly changing healthcare context, few studies have analysed the substance of master’s theses and their contribution to knowledge.
Norway has signed the Bologna Declaration, the intention of which is to promote the European system of higher education: a system of easily readable and comparable undergraduate and graduate degrees (21). In Norway, registered nurses (RNs) are required to hold a bachelor’s degree. Norwegian regulation on guidelines for the programs to become an intensive care nurse (ICN), operating room nurse (ORN) or nurse anaesthetist (NA) require 1.5 to 2 years post-graduate specialization (90 ECTS) or a master’s degree (120 ECTS) (22). According to the Norwegian Counsel of Nursing, there is an urgent need for master’s degree-level education to ensure clinical competence and functionality for nurses in the future (22). Yet there is an ongoing debate whether there is a necessity to complete the entire master’s program (120 ECTS). The new regulations from 2021 allow individuals to discontinue their studies after completing further education without having to write a full master’s thesis. To meet the growing call for master’s-degree competence in advanced practice, intensive care and operating room nursing, universities and university colleges have developed academic master programs (60 ECTS) through which ICNs, ORNs and NAs with 90 ECTS may advance to the master’s level (120 ECTS). Knowledge about who these students are, and their motivation to join the AMP, are sparse.
The academic master’s program (AMP)
To enable NAs and ICNs with a postgraduate education (90 ECTS) to attain a masters’ degree, this academic master’s program (AMP) was designed at a university in Norway (Figure 1):
- Theory and Value Foundation of Anaesthesia and Intensive Care Nursing with compulsory courses in Philosophy of Science and the Contextual Framework for Intensive Care Nursing (10 ECTS)
- Scientific Theory, Research Methodology, and Ethics (10 ECTS)
- Masters’ thesis project description (10 ECTS)
- Master’s thesis (30 ECTS)
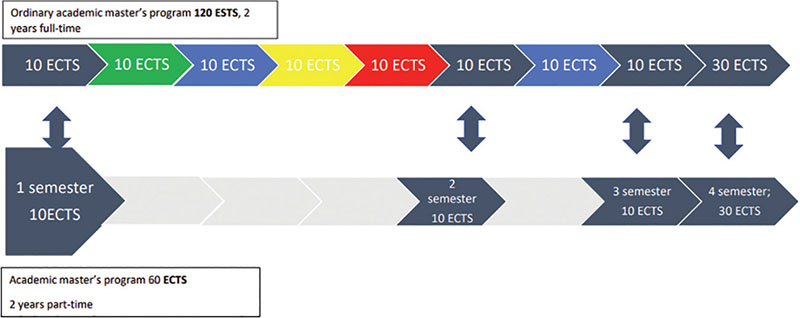
Figure 1 The AMP courses leading to a master’s degree in critical care nursing (120 ECTS) over four semesters
This study reports on the experiences of this new group of students in universities. The participants were all highly educated, with 90 ECTS in NAs and ICNs, and well-trained clinicians. This two-year, part-time AMP has proven popular: 10 to 15 students with postgraduate anaesthesia and intensive care nursing education and long experience within these specialties apply every second year, although the students work normal hours in the hospitals with no time off to study and little, if any, rise in pay after completing the AMP. This study aimed to explore and describe their motivation to enrol in an AMP at a university in Norway.
Methods
A qualitative, explorative, inductive design was chosen to gain a deeper understanding of what motivated the participants to enrol in the AMP. Focus groups (FGs) are a suitable method for exploring new areas with sparse knowledge (23) FGs are often preferred due to their explicit use of group interaction and discussions to produce data and insight that would be less accessible without the interaction found in a group (23). The COREQ checklist was followed, to ensure trustworthiness in the study (24).
Ethical considerations
The Norwegian Social Science Data Services approved the study (no. 23755). The participants were provided with information about the purpose and method of the study, that participation was voluntary, that they were free to withdraw at any time (25), that full confidentiality was ensured, and that all names would be removed from the transcripts. Then voluntary informed consents were signed by each participant in the focus group immediately before the interview took place. The participants were also asked for permission to audio record the interviews. To minimize a pressure to participate, a nurse manager from the hospital wards invited the participants to take part in the study.
Participants
All 16 NAs and ICNs with postgraduate education (90 ECTS) in intensive care nursing or anaesthetic nursing and extensive clinical experience, who had enrolled in the AMP at our university, received an open invitation to participate in this study. Eleven students accepted: two NAs and nine ICNs, and six among them hold leading positions in quality improvement. The interviews took place at the university during the second half of the AMP. Two FGs were organized, one with eight participants and one with three participants (Table 1). This uneven number was due to challenges we encountered regarding finding suitable times to meet. There was a discrepancy in NA and ICN participants, as fewer students with an NA background enrolled in the AMP.
| Participants | FG 1 | FG 2 |
|---|---|---|
| Male | 5 | 0 |
| Female | 3 | 3 |
| Total | 8 | 3 |
| ICNs | 7 | 2 |
| NAs | 1 | 1 |
| Leading positions in quality improvement | 5 (2 NA/3 ICN) | 1 (ICN) |
Data collection
A semi-structured interview guide with open questions was used to facilitate discussions in the FGs. The open questions invited participants to describe (a) what motivated them to enrol in the AMP and to (b) the value of the course in clinical practice through examples.
Both researchers, ICNs and connected to AMP, participated in the interviews, one as moderator and the other as observer. The researchers listened carefully and asked questions if necessary for clarification. All participants contributed and reported that they found the topic interesting to discuss. The participants were interviewed only once, face to face, with no one else present. The FGs had uneven numbers of participants: FG 1 had eight, while FG 2 had three (due to sick leave, only three of the five invited nurses took part). The interviews were audio recorded and transcribed by the first author. Neither the transcript nor the analysis of the transcripts was returned to participants for comments or feedback. The interviews were rich and regarded as having sufficient information power (26). Eleven participants described a broad variety of experiences from varied backgrounds, coming from different hospitals and wards, with different job experiences, in different life situations and with different systems to support them.
Data analysis
The interviews were analysed using an inductive approach (27). Immediately after each interview, the moderator (first author) and co-moderator (second author) met to discuss the interview process and content. The authors read the transcribed interviews and coded them separately (attachment analysis). Our individual understandings of similarities, differences and patterns were discussed in meetings and described in sub-categories and categories. As suggested by Graneheim (27), an effort was made to avoid presenting the categories and themes as classifications or general summaries; our aim was to capture the underlying meaning conveyed by the categories. The suggested sub-categories, categories, and the main theme were discussed in the research group.
Findings
In our investigation, we uncovered rich descriptions of participants’ motivation, which was tied to the overarching theme of improving patient care through continuous learning. The participants emphasized the critical role of continuous learning in delivering high-quality treatment and care to critically ill patients. However, a challenge emerged as the participants described a scarcity of time for learning within the demanding environment of busy wards, where effectiveness was prioritized as the primary goal. Consequently, participants found it necessary to step out of work in the wards and return to the university setting to facilitate their learning.
Three categories emerged, all reinforcing the central theme: understanding research; learning to argue effectively in interprofessional teams; enhancing the NAs and ICNs profession. Participants expressed a keen interest in comprehending the new knowledge generated by current research and actively participating in interprofessional discussions and implementation efforts aimed at enhancing treatment and care provision. They advocated for the integration of continuous learning into the daily life of the wards, emphasizing the potential to improve patient treatment and care.
Notably, participants reported a prevailing working culture that posed limited to no opportunities for learning. This finding underscores the challenge within the current professional environment, indicating a need for systemic changes to foster a more conducive learning culture.
Understanding research
Participants emphasized the significance of reading, comprehending, and critically reflecting on emerging scientific knowledge. They highlighted the value of sharing this knowledge with their professional teams for discussion. The academic master’s program (AMP) played an important role in equipping them with scientific methods and research terminology, essential tools for understanding research and fostering continuous learning. As a result, participants felt motivated to propose enhancements in care and the implementation of best practices.
In their own words, one participant described the impact of the program:
They introduce us to scientific articles to read … I am not completely there yet, but I am motivated to learn how to read and evaluate the article and not just read it and find it interesting. I want to be able to read it more “in depth” and understand what is behind here, to be able to evaluate the quality of, for example, these checklists: What are the benefits? (1.2)
This illustrates the participants’ eagerness to delve deeper into scientific literature and critically assess its relevance, showcasing a commitment to a more profound understanding of research concepts.
Participants expressed that the acquisition of new knowledge promoted self-reflection on their professional practices. The AMP provided them with tools to evaluate and enhance their own practices and bring this knowledge to the professional team for discussion, serving as a motivational factor.
In the words of one participant who holds a leading position in quality development in their Intensive Care Unit (ICU):
I am responsible for professional quality development in my ICU. We are obligated to work evidence-based (by law). I, therefore, need this competence to be able to do my job properly. This AMP teaches us to be a bit more “on the ball,” thinking in new ways. We’ve started to read research articles now and discuss them in the team. We’ve even thought about conducting some research in our department. We’ve started to discuss possible areas of improvements in our lunch breaks. Time will show what happens, but the motivation is there, at least. (2.1)
This highlights the participant’s recognition of the legal obligation for evidence-based practice and the role of the AMP in fostering innovative thinking and collaborative engagement within the team.
Participants observed a challenge in finding time for reflection and learning due to leaders prioritizing efficiency. The participants noted that leaders often focus on treating many patients to maximize revenue, neglecting the importance of learning and best practices as valuable investments. Despite a keen interest in learning during work, participants described the limited time available for activities like reading, discussing, or attending courses, attributing this scarcity to stringent budget constraints.
Leaders are interested in treating as many patients as possible in as short a time as possible, because that is how they earn their money. It is sad that they don’t regard learning and best practice as wise investments. I believe that improved treatment and care, reduction in errors and improved patient safety will save both money and human suffering. It is important to think in a broader perspective. (1.3)
We enjoy learning when working, but time is so short. Strict economy reduces opportunities for learning. Time to read, discuss or join a course is history—every little possibility to save money (in the short run) is used. (1.4)
We found that the value of learning was not solely framed as a professional obligation but also as a means of retaining experienced ANs and ICNs. Participants expressed that learning serves as a motivating factor that fosters a desire to stay in their roles. Additionally, they found satisfaction in being open to change and implementing new approaches, highlighting the positive impact of continuous learning on professional fulfilment.
Using scientific arguments in the interdisciplinary teams
Participants expressed a desire to contribute more effectively to interdisciplinary team discussions by using scientific arguments. They conveyed a motivation to enhance their competence and strengthen their ability to present compelling scientific arguments. Emphasizing the importance of building confidence, they believed that this confidence could empower them to speak up more assertively and be a more qualified participant in team discussions.
In the words of one participant:
I think being able to argue for the choices we make is even more important for me now. I believe it has been strengthened through this course. (2.1)
This statement reflects the participant’s acknowledgment of the heightened significance of effective argumentation and the perceived impact of the course on strengthening this skill.
The participant found the course particularly engaging. While initially more focused on the practical aspects of nursing, they expressed newfound excitement about delving into the philosophical aspects of science. This shift in perspective was attributed to the course’s emphasis on interprofessional collaboration in critical care settings.
Moreover, participants highlighted the motivational aspect of demonstrating that nurses have evidence-based practices. They expressed a desire to engage in discussions and arguments with physicians and management to improve the quality of treatment, care, and resource utilization. They believed that such proactive involvement would contribute to elevating the status of nurses within interprofessional teams.
The participants believed that the new knowledge gained from the course would not only enhance critical thinking but also improve patient care. They emphasized the importance of being able to argue for professional opinions, engage in research exploration, and actively participate in the ongoing development of professional knowledge.
I believe this new knowledge will improve patient care—the critical thinking, being able to argue for your professional opinions, search for new research and participate in the further development of professional knowledge. (2.1)
For those working with procedures and guidelines, the course provided a sense of accomplishment. Learning how crucial it is to base these procedures on the best evidence and gaining advanced skills in reading, understanding, and reflecting on research contributed to a heightened sense of professional satisfaction.
Because I work with procedures and guidelines, it feels good to learn how important it is to base them on the best evidence and to learn how to do it. It feels good to be able to read and understand and reflect on research in a more advanced manner than before. (1.2)
Participants expressed optimism about bringing a renewed enthusiasm to anaesthetic and ICU-departments as they applied their newly acquired academic knowledge in their work. Some had already initiated discussions and proposed changes with their leaders. Additionally, they emphasized the positive impact of continuous learning, critical reflection, and interprofessional discussions on various aspects of their professional lives, including working conditions, career planning, and the retention of NA and ICN.
One participant voiced a common sentiment:
I believe that those criticizing NAs and ICNs with master’s degrees do not know what it is all about. They believe it is all about writing a thesis. They do not know all the things we learn through this AMP. I feel that I must tell them and argue for the importance of this kind of knowledge. (1.4)
This statement underscores a perceived misunderstanding, that the AMP in solely involving thesis writing.
Furthermore, participants expressed a belief that undertaking the AMP leads to an elevated level of understanding, making individuals better practitioners. One participant stated:
I believe that you do become a better practitioner by taking the AMP because you understand more on a higher level. (1.5)
The participants acknowledged a concern among leaders that obtaining a master’s degree might lead to professionals leaving hospitals to work at universities. Despite this concern, leaders were perceived as reluctant to invest adequately in retaining. This reflects a tension between the desire to retain skilled professionals at the bedside and the need for recognizing and supporting their advanced education and expertise, as expressed in the statement:
Our leaders are afraid that we will leave the hospitals when we get our master’s degree and start working at the university. They want to keep us bedside, but they do not pay the price. (2.3)
Discussion
This study aimed to explore and describe what motivated NAs and ICNs to return to university and enrol in an AMP. We found that their need to continuously learn, in order to improve patient care, was central. The participants wanted to be engaged in a learning process. They wanted to be able to understand and discuss relevant research in the inter- and intraprofessional teams and use new knowledge bedside to improve treatment and care. In acute wards, the development of techniques, treatment and caring procedures must follow new research being rapidly disseminated and requires continuous learning and improvement of professional and personal competence. However, the participants described time to learn and discuss when working as nearly non-existent. Consistent with Goldsworthy’s (28) findings, we observed that when workload is high, quality improvement and interprofessional learning are frequently deprioritized, often due to cost-saving measures. This may explain the NAs’ and ICNs’ constant desire for new knowledge.
Investment in continuous learning and professional development
We found that, with little or no time for learning and reflection in the wards, the participants in this study had to search for learning opportunities outside of the hospitals. By bearing the cost of the AMP themselves, participation in the AMP was a personal investment in the nurses’ own career development, with no financial ties to their previous workplace. Completing the AMP may also increase their market value outside the hospitals. At a time when it is crucial to retain and recruit highly qualified nurses in hospitals, the availability of educational opportunities in hospitals at all stages of a nurse’s career may prove paramount (29). By prioritizing professional development, hospitals can promote nurse retention within critical care units, potentially stabilizing the workforce and helping with nurse recruitment (28). The availability of professional development, or educational opportunities, has also been linked to characteristics of a healthy work environment that both attracts and retains nurses (30).
The participants highlighted the value of the AMP, as the knowledge they acquired is crucial in specialized wards, where new research-based information is disseminated from a diverse range of data sources on a daily basis. They expressed the need to be able understand, critically reflect on, and discuss the studies and results in a professional way in the interprofessional teams, to improve patient care. We believe that this is an underestimated need, in line with Hansen and Dysvik (13).
More qualified decisions
The participants described a desire to make more qualified decisions in patients’ care as a motivational factor to enrol in the AMP. This is in line with Cotterill-Walker’s (31) and Skogsaas and Valeberg’s (15) findings, which describe how academic competence inspired the nurses in their studies to bring relevant research into daily discussions and rounds in the ICUs. This allowed them to affect patient care by performing more competent EBN. Some participants in the present study described standards and protocols in their own wards as being outdated and were eager to make them evidence based to improve patient safety. The participants were highly motivated to further develop their professional knowledge, in order to give patients the best possible care by applying newly acquired information. They wanted to take part in the inter- and intraprofessional team discussions and be included as a qualified member of the team. Professional development in nursing, like the AMP, increases confidence and self-esteem, enhances communication, promotes personal and professional growth, deepens knowledge and application of theory to practice, and improves analytical/critical thinking and decision making (19,31) and turns the nurses into advanced practitioners and qualified team members.
Drive to learn and develop new knowledge
The participants found enjoyment and motivation in the learning process—particularly in gaining the ability to understand and use scientific arguments in interprofessional discussions and striving for excellence and growth. Despite their extensive experience as NAs and ICNs, they expressed a need for competence in EBN, in order to be able to provide safer, more confident care in their everyday practice. They described their professional motivation as, in part, driven by a fear of being compared to younger and more competent ICNs.
The research-based master’s thesis the participants wrote as a part of the AMP represented a valuable contribution not only to the course participants. In line with Hansen and Dysvik (13), they developed new knowledge within each profession. The thematic foci of these theses were clinically directed, determined through input and discussion from the clinical field. We believe that academic competence in research methods and theory of science and nursing is required to understand the theoretical aspects within any specialist field in nursing—and, moreover, stimulates the continuous learning process. In addition, and in accordance with Hansen and Dysvik (13), we argue that it is important to understand and generate new clinical knowledge and to be able to initiate new research projects. Professional development may also improve career development, supplement gaps in prior education, give relief from routine, build professional networks and optimize patient care (19,31).
The prevailing ideology in healthcare services, New Public Management, prioritizes cost efficiency over all other considerations, aiming to provide the most effective healthcare services at the lowest price (32). Despite the high workload resulting from this approach, the participants retained the urge to learn. They felt stimulated by the AMP and had already begun to disseminate their new knowledge to their colleagues and plan small improvement projects. Our findings also highlight the significance of continuing the learning process beyond the conclusion of the AMP. Here, participants underlined the importance of having support from their leaders and colleagues, in which they noted large variations. Some participants reported that their leaders exhibited limited acknowledgement of the positive impact that ongoing learning can have on cognitive abilities related to systems and processes. In line with Abu-Qamar et al. (33), continuing learning promotes a more stable work force, reduces turnover, enhances mentorship opportunities, and increases awareness of the organizational culture. While the impact of continuous learning activities on quality nursing care can be challenging to measure, we posit that the effects may become apparent in the long-term budgets through improved patient safety and job satisfaction.
Different applications
For some participants, one motivating factor for enrolling in the AMP was the belief that it would increase their employability on the job market. Most of the participants believed that their master’s thesis and the academic competence they had acquired improved not only their qualifications but also their ability to speak up, reflect and argue on a higher level—and they regarded this competence as valuable. Most participants, however, reported that their main motivation for enrolling in the AMP was to increase their competence in their present jobs. They wanted to improve the learning culture in their workplace, to close gaps in their prior education, to increase their self-esteem, to do something new, to build a professional network and to improve healthcare, in line with the findings of Cotterill-Walker (31) and Pool et al. (19). The participants described increased confidence and self-esteem, enhanced communication, personal and professional growth, knowledge, application of theory to practice, and analytical thinking and decision making as important skills to improve nursing.
Trustworthiness
The first steps of the analysis process were undertaken separately. To ensure credibility of the analysis, the identified meaning units, codes and categories were discussed by both researchers. By presenting statements from the participants in this article, credibility has been strengthened. Transparency was maintained throughout the process, with descriptions of every step taken in the data collection and analysis process. All text from the transcripts was read by both researchers to assess comparability with the codes, categories and themes identified. Transferability was attended to by describing the context, the reflectivity, and every step of the research process. Dependability was ensured by using the same interview questions for all participants; it was also strengthened by the researchers’ experience as ICNs in clinical practice and from the university. Both authors participated in the FG, with the first author as moderator and second author as observer. Some limitations of trustworthiness might occur because both researchers have relations with the participants. The FGs dialog, and even the analysis and findings, might be influenced by this connection.
Conclusion
Improving patient care for the critically ill through continuous learning was the primary motivating factor for NAs and ICNs to enrol in the AMP. However, time to learn was described as scarce in very busy wards, where effectiveness was regarded as the most important goal. We found that academic knowledge equipped the participants with the necessary tools with which to understand research, effectively argue their viewpoints within interdisciplinary teams and improve and develop the advanced nursing professions. A constant need for learning motivated NAs and ICNs to enrol in the AMP with little or no support from the hospitals. The finding that NAs and ICNs desire continuous learning is relevant for hospital leaders who struggle to achieve patient safety goals and retain/recruit highly competent advanced nurses.
Funding statement
There was no founding source involved with this study.
Declaration of competing interest
None.
References
- 1. Knap M, Ozga D, Krupa S, Penar-Zadarko B, Mędrzycka-Dąbrowska W, Witt P, Friganovic A. Position statement of the European Specialist Nurses Organisation (ESNO) in specialist nursing as advanced practice nursing towards 2030. Pielegniarstwo XXI wieku/Nursing in the 21st Century. 2020;19(4):274-80. https://doi.org/10.2478/pielxxiw-2020-0032
- 2. World Health Organization. European strategic directions for strengthening nursing and midwifery towards Health 2020 goals [Internet]. Geneva: WHO; 2015. Available from: https://apps.who.int/iris/
- 3. Abraham PJ, La Donna D, Pfrimmer DM. Retaining master and DNP registered nurses in direct patient care: utilizing nurses to the fullest extent of their education. Nurse Lead. 2015;13(1):70-4. https://doi.org/10.1016/j.mnl.2014.05.019
- 4. Fulbrook P, Albarran JW, Baktoft B, Sidebottom B. A survey of European intensive care nurses’ knowledge levels. Int J Nurs Stud. 2012;49(2):191-200. https://doi.org/10.1016/j.ijnurstu.2011.06.001
- 5. Hellesø R, Fagermoen MS. The contribution of research-based master’s theses to knowledge building in nursing. J Nurs Educ Pract. 2018;8(11):35-42. http://dx.doi.org/10.5430/jnep.v8n11p35
- 6. King R, Taylor B, Talpur A, Jackson C, Manley K, Ashby N, et al. Factors that optimise the impact of continuing professional development in nursing: a rapid evidence review. Nurse Educ Today. 2021;98:104652. https://doi.org/10.1016/j.nedt.2020.104652
- 7. Massimi A, Marzuillo C, Di Muzio M, Vacchio MR, D’Andrea E, Villari P, De Vito C. Quality and relevance of master degree education for the professional development of nurses and midwives. Nurse Educ Today. 2017;53:54-60. https://doi.org/10.1016/j.nedt.2017.04.012
- 8. McGhie-Anderson R. Advanced nursing education: Critical factors that influence diploma and associate degree nurses to advance. Florida: Barry University School of Nursing; 2016.
- 9. Millberg LG, Berg L, Brämberg EB, Nordström G, Öhlén J. Academic learning for specialist nurses: a grounded theory study. Nurse Educ Pract. 2014;14(6):714-21. https://doi.org/10.1016/j.nepr.2014.08.008
- 10. Mlambo M, Silén C, McGrath C. Lifelong learning and nurses’ continuing professional development, a metasynthesis of the literature. BMC Nurs. 2021;20(1):1-13. https://link.springer.com/article/10.1186/s12912-021-00579-2
- 11. Gerard SO, Kazer MW, Babington L, Quell TTJ. Past, present, and future trends of master’s education in nursing. J Prof Nurs. 2014;30(4):326-32. https://doi.org/10.1016/j.profnurs.2014.01.005
- 12. Palese A, Zabalegui A, Sigurdardottir AK, Bergin M, Dobrowolska B, Gasser C, et al. Bologna process, more or less: nursing education in the European economic area: a discussion paper. Int J Nurs Educ Scholarsh. 2014;11(1):63-73. https://doi.org/10.1515/ijnes-2013-0022
- 13. Hansen BS, Dysvik E. Value of research-based master’s degree theses. Inspira. 2022;17(1). https://doi.org/10.23865/inspira.v17.3156
- 14. Alshahrani HH. Evaluating the impact of continuing professional development within intensive care unit nurses in the UK. Am J Nurs. 2020;8(2):227-44. https://doi.org/110.12691/ajnr-8-2-12
- 15. Skogsaas B, Valeberg BT. The contribution of a master’s degree to clinical practice. Norwegian Journal of Clinical Nursing/Sykepleien Forskning. 2017;12(63495):e-63495. https://doi.org/10.4220/Sykepleienf.2017.63495en
- 16. Amundsen G, Karlsen H, Lid S. Underviserundersøkelsen 2021 [Internet]. Oslo: NOKUT; 2021. Available from: https://www.nokut.no/globalassets/studiebarometeret/underviserundersokelsen/underviserundersokelsen-2021_hovedrapport_10-2021.pdf
- 17. Henriksen KF, Hansen BS, Wøien H, Tønnessen S. The core qualities and competencies of the intensive and critical care nurse, a meta-ethnography. J Adv Nurs. 2021;77(12):4693-4710. https://doi.org/10.1111/jan.15044
- 18. Stafseth SK, Tønnessen TI, Diep LM, Fagerstrøm L. Testing the reliability and validity of the nursing activities score in critical care nursing. J Nurs Meas. 2018;26(1):142-62. https://doi.org/10.1891/1061-3749.26.1.142
- 19. Pool IA, Poell RF, Berings MG, Ten Cate O. Motives and activities for continuing professional development: an exploration of their relationships by integrating literature and interview data. Nurse Educ Today. 2016;38:22-8. https://doi.org/10.1016/j.nedt.2016.01.004
- 20. Ross K, Barr J, Stevens J. Mandatory continuing professional development requirements: what does this mean for Australian nurses. BMC Nurs. 2013;12(1):1-7. https://bmcnurs.biomedcentral.com/articles/10.1186/1472-6955-12-9
- 21. Marquand J, Scott P. The Bologna Declaration of 19 June 1999. In: Marquand J, ed. Democrats, authoritarians and the Bologna process. Leeds: Emerald Publishing; 2018. pp. 183-86. https://doi.org/10.1108/978-1-78743-439-420181009
- 22. Forskrift om nasjonale retningslinjer for intensivsykepleierutdanning. FOR-2021-10-26-3094. Available from: https://lovdata.no/LTI/forskrift/2021-10-26-3094
- 23. Brinkmann S, Kvale S. Doing interviews (Vol. 2). London: Sage; 2018.
- 24. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-57. https://doi.org/10.1093/intqhc/mzm042
- 25. World Medical Association. The declaration of Helsinki [Internet]. Geneva: World Medical Association; 2004. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
- 26. Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753-760. https://doi.org/10.1177/1049732315617444
- 27. Graneheim UH, Lindgren B-M, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurs Educ Today. 2017;56:29-34. https://doi.org/10.1016/j.nedt.2017.06.002
- 28. Goldsworthy SJ. The mechanisms by which professional development may contribute to critical care nurses’ intent to stay [PhD dissertation]. Vancouver: University of British Columbia; 2015. http://hdl.handle.net/2429/52672
- 29. Lavoie-Tremblay M, Wright D, Desforges N, Gélinas C, Marchionni C, Drevniok U. Creating a healthy workplace for new-generation nurses. J Nurs Scholarsh. 2008;40(3):290-97. https://doi.org/10.1111/j.1547-5069.2008.00240.x
- 30. Salehi T, Barzegar M, Yekaninejad MS, Ranjbar H. Relationship between healthy work environment, job satisfaction and anticipated turnover among nurses in intensive care unit (ICUs). Ann Med Health Sci Res. 2020;10(2).
- 31. Cotterill-Walker SM. Where is the evidence that master’s level nursing education makes a difference to patient care? A literature review. Nurs Educ Today. 2012;32(1):57-64. https://doi.org/10.1016/j.nedt.2011.02.001
- 32. Peyton MM. New Public Management in health care its effects and implications [Thesis proposal]. Aarhus School of Business, Aarhus University Denmark. Aarhus: Aarhus University; 2009.
- 33. Abu-Qamar M, Vafeas C, Ewens B, Ghosh M, Sundin D. Postgraduate nurse education and the implications for nurse and patient outcomes: a systematic review. Nurs Educ Today. 2020;92:104489. https://doi.org/10.1016/j.nedt.2020.104489