Introduction
Intensive care units (ICUs) have become an area of increased specialization with very ill patients and advanced technology (1). Nurses and critical care nurses (CCN) are in shortage worldwide, which is worsened by the large numbers of experienced nurses and CCNs nearing retirement, resulting in recruitment problems (2). In Europe, Aiken et al. (3) found an association between nurse workload and postoperative mortality. Increased care quality and improved work environment were associated with reduced ratios of patients to nurses in Europe and the United States (4). The basis of nursing, especially critical care nursing, is education, with both individual skills and competencies (2). Competence is often defined as “the ability of a nurse to demonstrate the knowledge, skills, judgment and attitudes required to perform activities within the defined scope of practice at an acceptable level of proficiency” (5). Inter-professional collaboration and competence within a team are necessary for patient safety, with the ideal being “right profession, right number at [the] right place” (6,7).
National and international guidelines for the levels of qualified nursing staff in critical care are based on the opinions of expert groups and produced by various nursing and medical professional bodies in many countries (1). Advanced competence in intensive and critical care nursing (ICCN) is a multidimensional concept, and evaluations of education and competence within this field are important (8). Doran et al. (9) described the nursing role effectiveness model and reformulated the concept using nurse-sensitive indicators, nursing performance quality indicators, or outcomes potentially sensitive to nursing (9,10). Nurse-sensitive outcomes are “those that are relevant, based on nurses’ scope and domain of practice, and for which there is empirical evidence linking nursing inputs and interventions to the outcomes” (6). Moreover, if the outcome deteriorates, it is within the aspect of patient safety. Previous reviews have focused on the impact of nurses in critical care and patient outcomes (6), while Gill et al. (11) focused on nursing staffing, education, and practice standards. An important review by Greaves et al. described nursing workload and activity in critical care, with validated tools but without a presentation of patient outcomes (1). There is a lack of up-to-date reviews focusing on the relationship between nurses’ characteristics such as level of competence, nurse staffing, and patient outcomes.
In Norway, registered nurses (RNs) are required to hold a bachelor’s degree. Becoming a CCN requires 1.5–2 years of further post-graduate specialisation. Critical care is affected by the nursing shortage. The state of ICU staffing has been mapped in a national Norwegian study that involved 62 ICUs (67.7% return rate) and described a high age profile of nurses and a nurse-to-patient ratio of 1:1 to 2:1 (12).
AIM
The aim of this scoping review was to obtain an understanding of how nursing competence and staffing in ICUs are described, applied, and associated with nurse-sensitive outcomes. The review questions were as follows:
- How is nursing competence in ICUs described?
- How is nurse staffing described, applied, and measured?
- How are nurse competence and staffing in ICUs associated with nurse-sensitive outcomes?
Methods
Study design
A scoping review was conducted to present a descriptive overview of findings without synthesizing evidence from different studies (13–15). Scoping of the most current critical care nursing literature and the development of instruments for measuring nursing workload increased in use after 2005. Therefore, the search limits were set for articles published between 2006 and May 2023. CINAHL, Medline, Embase, the British Nursing Index, and SweMed+ were searched for suitable primary research studies with a quantitative design in English. A comprehensive search strategy was used to identify published studies by using the keywords “acute care”, “infection control”, “length of stay”, “treatment errors”, “adverse health-care event”, “adverse events”, “skill mix”, “personnel staffing and scheduling”, “critical care nursing”, “clinical competence”, AND/OR “risk management”. The Medline search strategy is presented in Appendix I. The search was adapted for each subsequent database.
Study selection
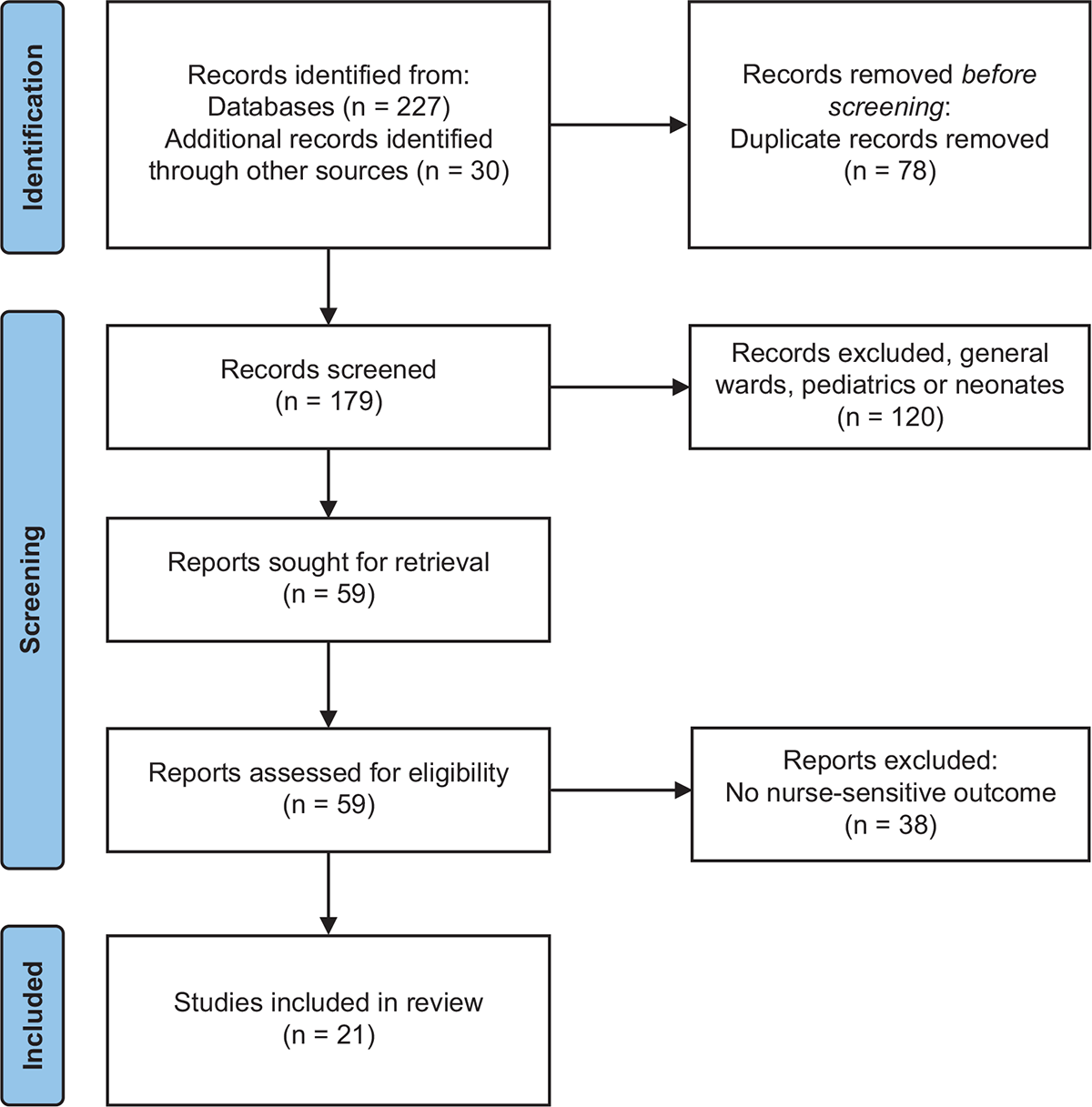
The articles included in this review met the following criteria: peer-reviewed articles available in full text, primary research, studies published in English or Scandinavian language, studies that focused on nurses working in critical/intensive care and nurse-sensitive outcomes for ICU patients. Studies that focused on general nursing or on specific groups such as neonates or paediatric patients were excluded (Figure 1). This review study is reported in accordance with the PRISMA 2000 checklist. The titles and abstracts of the included studies were independently assessed by two of the authors for eligibility against the inclusion and exclusion criteria and categorized as “possibly relevant” or “clearly not relevant”. This process was repeated with full-text studies. New references were found and followed the same stages for the inclusion process (Table 1). Only small disagreements occurred and were discussed in the research group until consensus was reached. The quality assessment based on the Critical Appraisal Skills Programme (CASP) checklist was independently performed by two authors.
Ethical considerations
This is a literature review, and no approval is required. All included studies had clearly identified ethics.
Results
The scoping review included 21 studies from different countries (Table 1). The studies were published in both nursing (13 articles) and multi-disciplinary journals (8 articles). Of the studies, 2 were randomized controlled trials (RCTs), 11 were retrospective studies, and 8 were prospective observational studies. The sample sizes ranged from 79 to 38,162 patients in ICUs. Other studies focused on ICUs in single- to multi-centre studies, with a total of 171 ICUs. Four studies included both wards and ICUs, analysed separately. In the included studies, nurse-sensitive outcomes were defined as nosocomial infections (i.e. catheter-associated urinary tract infections, central line-associated blood stream infections, and ventilator-associated pneumonia) (16–22), decubitus ulcers (19), adverse drug events (ADEs) (19,23–24), dislodgement of tubes (cannulas, lines, and drains) (23,25), length of hospital stay (20,25–28 ), and mortality (20,26,29–34).
| Author and year, (ref) journal, country | Aim | Study design and sample characteristics | Competence | Nurse staffing (ratio), and tools | Nurse-sensitive outcome | Key points/comments |
|---|---|---|---|---|---|---|
|
Blatnik J et al., 2006 (36) Journal of Hospital Infection Slovenia |
To investigate the correlation between daily workload of nurses and the spread of infection caused by methicillin resistant Staphylococcus aureus. | Prospective observational study (three years), 297 patients in one surgical ICU. | A professionally qualified and experienced nurse in an ICU. | Therapeutic intervention scoring system (TISS), one nurse can achieve 40 TISS points. One nurse covered the workload of two nurses. | Infections | Work overload (TISS) of nurses were an important risk factor for the spread of nosocomial infections. |
|
Dancer SJ et al., 2006 (21) American Journal of Infection Control Scotland |
To investigate methicillin-resistant Staphylococcus aureus acquisition and association with nurse staffing levels. | Retrospective observational study (five months), 174 patients in one 8-bed ICU. | Nurse staffing levels for trained, agency, and auxiliary nurses (both day and night duties). | Patient dependency scores modified Therapeutic Intervention Scores (TIS), and trained nurses. | Infections and hygiene failures. | This results suggests that patient acquisitions of infections were 7 times more likely during periods of understaffing. |
|
Hugonnet S et al., 2007A (22) Critical Care Medicine Switzerland |
To determine whether low staffing level increases the infection risk in critical care. | Prospective observational, single-center cohort study (four years), 1,883 patients, medical ICU. | Nurses certified in critical care divided by the number of nurses in training. | Projet de Recherche en Nursing (PRN) for estimation the required nursing staff for each shift in nurse per hour. | Nosocomial infections, occurrence of ICU-acquired infection; pneumonia. | Low nurse staffing is associated with an increased 50% infection risk, and a substantial proportion of all infections acquired in critical care could be prevented, by maintaining staffing at a higher competence level. |
|
Hugonnet S et al., 2007B (18) Critical Care Switzerland |
To explore workload and infection risk of ventilator associated pneumonia (VAP) in critically ill patients on early and late onset. | Prospective observational study (four years), 2,470 patients on mechanical ventilation in a single-center medical ICU. | Nurse training level and a model of nurse to patient ratio. |
Projet de Recherche en Nursing (PRN) for estimation the required nursing staff for each shift. Total numbers of nurses working divided by the patient numbers/ 24-hr Nurse per hour. Nurse to patient ratio; ≤1.8, 1.8 to ≤1.9, 1.9 to 2.2, and >2.2 |
Late onset VAP was six days after intubation. | High nurse per hour associated with a decreased risk for late-onset VAP. Adequate staffing is a prerequisite for high-quality care and patient safety. |
|
Tourangeau AE et al., 2007 (31) Journal of Advanced Nursing Canada |
To explore the nursing-related determinants of risk-adjusted 30-day mortality for acute medical patients in hospitals. |
Retrospective observational study (one year), 46,993 medical patients (both general wards and ICUs, in 75 hospitals. | RN | Proportion of RN staffing and nurse reported staffing adequacy. | 30-day mortality | Lower mortality associated with higher proportion RN and adequacy of staffing. |
|
Cho S-H et al., 2009 (34) Nursing Research Korea |
To examine the relationship between nurse staffing and patient mortality. | Retrospective observational study, 27,372 patients in 42 tertiary and 194 secondary hospitals ICUs. | RN and nurse experiences. | Ratio of average daily number nurses (census) to total number RN in full-time equivalents. | Mortality | Additional patients per RN associated with increased odds ratio for mortality. Not significant for nurse experiences. |
|
Kiekkas P et al., 2008 (29) Journal of Nursing Scholarship Greece |
To investigate mortality of ICU patient between the ratios of nurse staffing and total patient care demands. | Prospective observational study (one year), 396 medical and surgical patients in one ICU. |
Registered and licensed practical nurses. Nurse experiences >5 years. |
Therapeutic intervention scoring system (TISS-28) was calculated daily. | Mortality | It was a positive trend in increased mortality with increased workload (not significant). |
|
Sales A et al., 2008 (32) Medical Care Canada |
To evaluate the association of in-hospital patient mortality with registered nurse staffing and skill mix. | Retrospective observational study, 129,579 patients from 171 ICU and 282 non-ICU in 123 hospitals. | RN, licensed practical nurse and nurse aide. | RN hours per patient day, RN skill mix as the proportion of total nursing hours provided by RNs, where total nursing hours included licensed practical nurse and nurse aide hours of care. | Mortality | Nil significant association found between ICU staffing levels and mortality. |
|
Kendall-Gallagher D et al., 2009 (19) American Journal of Critical Care USA |
To explore the relationship between the proportions of certified staff nurses in a unit and risk of harm to patients. | Correlational, cross-sectional of secondary analysis of 48 ICUs (one year), from a random sample of 29 hospitals. | Magnet status, Nurse certification, education, experience, skill mix. | Total hours of nursing care per patient and day. | Medication administration errors, total falls, skin breakdown, nosocomial infections: central catheter, urine tract and bloodstream infection. | A relationship between unit proportion of certified nurses and patients’ outcomes were detected but varied by outcome and direction of relationship. |
|
Van den Heede K et al., 2009 (33) International Journal of Nursing Studies Belgium |
To examined the association between nurse-staffing levels in postoperative cardiac surgery patients and mortality. | Retrospective observational study (one year), 9,054 cardiac surgery patients in 58 ICUs and 75 general nursing units. | Nurses and RN with a Bachelor’s degree. | Nurse staffing levels i.e. acuity-adjusted Nursing Hours per Patient Day (NHPPD), the proportion of Nursing hours per patient. | Mortality in three models. | Nurse-staffing variables had no significant impact on mortality. A greater number of NHPPDs in postoperative general nursing units were associated with lower mortality in all three models. |
|
Seynaeve S et al., 2010 (24) American Journal of Critical Care Belgium |
To assess the characteristics of adverse drug events in ICU and determine the impact of severity of illness and nursing workload on the prevalence of the events. | Retrospective, cross sectional survey (5 months), 79 patients in 1009 hospitals days (3,027 shifts), in medical and surgical ICUs. | Nurses or ICU-nurse. | Therapeutic intervention scoring system (TISS-28) Night: 2 nurses to 6–7 patients, late evening 3 nurses and 5 to 6 in the morning. | Adverse drug events, also in transport of patients. | 230 adverse drug events occurred in 79 patients, AEs were associated with illness severity and nursing workload. |
|
Blot SI et al., 2011 (16) American Journal of Critical Care Europe |
To determine the patient to nurse ratio and risk for Ventilator associated pneumonia (VAP). | Secondary analysis of a cohort 2,585 consecutive patients on mechanical ventilation. Retrospective observational study, 1,658 patients from 27 ICU in 9 European countries. | RN and ICU nurses: generally qualified to manage ventilator (use of respiratory therapists is rare). Unit-based standard nurse staffing levels irrespective of acute staff shortages. | For units with variable staffing the highest patient to nurse ratio in 24 hours period was considered. | VAP | Nurse to patient ratio 1:1 appeared to associate with a lower risk for VAP. Did not adjust for knowledge, and or for competence in ICU nurses with ventilator competence. |
|
Daud-Galotti RM et al., 2012 (17) Plos One Brazil |
To evaluate the role of nursing workload in the occurrence of Hospital associated infections (HAI). | Prospective observational study (three months), 195 patients in three medical ICU and one step-down unit. |
Healthcare workers (HCW): RN or technician |
Nursing activities score (NAS). The ICUs have one HCW for 2 beds, and in the step-down unit this proportion is of 3–4 beds per HCW. | HAI | Only excessive workload for HCW and severity of patient’s clinical condition remained as risk factors to HAI. |
|
Moneke N et al., 2013 (35) Journal of Nursing Administration USA |
To explore the factors influencing critical care nurses’ perception of their job satisfaction. |
Correlational survey of 224 critical care nurses (CCN) in 6 ICUs all specialized. (n = 129 in the analysis). |
Level of education; Bachelor in nursing (73), Master’s in nursing (23). Certification (n = 59), CCRN (55), Cardiac Medicine Certificate = CMC (4) |
Not in the study. The Leadership Practices Inventory (LPI) instrument and the Job in General scale (JIG). |
Job satisfaction | The leader must be clear about his/her personal leadership philosophy. Leaders should establish patterns of interaction that help their followers to work collaboratively to achieve patient outcomes. |
|
Thompson DA et al., 2013 (20) Journal of Nursing Care USA |
To assess the effects of nursing care hours per day and nurse sensitive outcomes. |
Longitudinal randomized control, intervention study of 45 ICUs in 35 hospital in12 states (2007–2008). Intervention: improving patient safety, teamwork and interdisciplinary communication. |
RNs and unlicensed assistive personnel (UAP). |
The level of nurse staffing was estimated nurse care hours per patient day. Nurse turnover. The Practice Environment Scale of the Nursing Workforce Index (PES-NWI) measured the job-satisfaction and quality of nursing care delivery. |
Length of stay (LOS), central line associated blood stream infections (CLABSI) and mortality. | A higher skill-mix was associated with LOS. Nurse care hours per day greater than 20 hours was associated with lower CLABSI. Relationship of nursing turnover with any outcome was not significant. |
|
Valentin A et al., 2013 (23) Intensive Care Medicine Austria |
To assess medication and dislodgement errors. | Prospective observational, cross-sectional study (48 Hours), in 57 intensive care units (ICUs) in three countries (Austria, Germany, and Switzerland). | Nurse, front line staff | Nurse to patient ratios and physician-patient ratios calculated by dividing “total working time”, mean number of respective staff multiplied with 48 h by “bed usage”, (sum of all hours of patient observation). Nursing Manpower Use Score (NEMS). Vienna Safety Climate Questionnaire (VSCQ). | Medical errors | Safety climate apparently contributes to a reduction of medical errors that represent a particularly error-prone aspect of frontline staff performance in intensive care. |
|
Lucchini A et al., 2014 (28) Intensive and Critical Care Nursing Italy |
To analyze workload, length of stay (LOS) and risk of developing pressure ulcers. | Retrospective observational study (5 years), 5,856 patients in three intensive care units (general, neurosurgical and cardiothoracic). | Nurses in ICU. |
A nurse to patient ratio estimated at 0.6. Number of nurses for each active ICU bed. Nurses are allocated regardless of the level for patient severity. Nursing Activities Score (NAS). |
Length of stay (LOS) and risk of pressure ulcers. |
The NAS was high in patients with increasing LOS (p < 0.003). The NAS does not seem to be linked to the risk of developing pressure ulcers. |
|
West E et al., 2014 (30) International Journal of Nursing Studies United Kingdom |
To investigate whether the size of the workforce (nurses, doctors and support staff) has an impact on the survival chances of critically ill patients both in ICU and in the hospital. | Retrospective observational study (6 months in 1998), cross-sectional risk adjusted, 38,168 patients in 65 ICUs. |
Nurses in direct care and super numerary nurses. Skilled nurses. |
The number of direct care nurses per bed and the number of supernumerary nurses. | Mortality; ICU and hospital. |
Association between the number of nurses and doctors available in ICU and patients’ chances of survival. The size of the nursing workforce had the greatest effect on the most severely ill patients in the ICU. |
|
Lærkner E et al., 2016 (27) Nursing in Critical Care Denmark |
To investigate nursing workload in and no-sedation with a group of sedated patients with daily wake up. | Randomized control trial (RCT), (21 months) in 140 patients from general ICUs. | Nurses perform dialysis, mobilization and weaning of mechanical ventilator. | The policy to have nurse to patient ratio 1:1 to sedated patients compared to 1:2 to non-sedated. Nursing Care Recording System (NCR11). | Length of stay (LOS). | A shorter ICU stay and shorter hospital length of stay in the no-sedation group. No differences in workload. |
|
Falk A-C et al., 2016 (25) Intensive and Critical Care Nursing Sweden |
To identify and evaluate the specialist nurse role for the quality of patient care in general ICUs. | Retrospective observational study (in 2010–2014), 33,032 patients at general ICU in University hospitals. |
Specialist nurse in critical care; 3 years (bachelor degree) plus an additional one-year for advanced level (Master degree). Nurse assist. |
Nurse-patient ratio of 0.5, or 0.6, or 1:1. Nurse assist per patient 0.1-0.5:1. | Hospital length of stay, ICU length of stay, unplanned extubations and time on mechanical ventilator. |
Hospital length of stay and time on ventilator was found; in hospitals with the least amount of patients and with 0.5-0.6 Specialist nurse-patient ratio. Lower nurse- patient ratio showed longer length of ICU stay. |
|
Jansson et al., 2020 (26) Journal of Advanced Nursing Finland |
To determine whether nurse staffing and nursing workload are associated with multiple organ failure and mortality. | Retrospective observational study (in 2008–2017), 10,230 patients at mixed medical-surgical ICU in tertiary-level teaching hospital. | Nurses in ICU | Therapeutic intervention scoring system (TISS-76) 40–50 points = 1 nurse, and Intensive care nursing scoring system (ICNSS) per nurse to patient ratio 1:1 ≤ 32. | Multiple organ failure and mortality. | Increased nursing workload are associated with multiple organ failure and mortality. |
| Author/year (ref) | Criteria of scoping Conceptual clarification of topic and definitions | Type of publication:
N = Nursing journal, M = Multi-disciplinary journal |
Design/method: NS = Non-systematic lit review, P = Prospective, R = Retrospective, O = Observational and nonexperimental design, C = Correlational, RCT = Randomized Control Trial | Identification of strengths and weaknesses of research base | Identification of research gaps and recommendations for further research | Implication for clinical practice | Ethics |
|---|---|---|---|---|---|---|---|
| Blatnik J et al. 2006 (36) | clearly identified | M | O, R | clearly identified | clearly identified | clearly identified | clearly identified |
| Dancer SJ et al. 2006 (21) | clearly identified | M | O, R | clearly identified | clearly identified | not cleary identified | clearly identified |
| Hugonnet S et al. 2007A (22) | clearly identified | M | O, P | clearly identified | clearly identified | clearly identified | clearly identified |
| Hugonnet S et al. 2007B (18) | clearly identified | N | O, P | clearly identified | clearly identified | clearly identified | clearly identified |
| Tourangeau AE et al. 2007 (31) | clearly identified | N | O, R | clearly identified | clearly identified | not clearly identified | clearly identified |
| Cho S-H et al. 2009 (34) | clearly identified | N | O, R | clearly identified | clearly identified | not clearly identified | clearly identified |
| Kiekkas P et al. 2008 (29) | clearly identified | N | O, P | clearly identified | clearly identified | clearly identified | clearly identified |
| Sales A et al. 2008 (32) | clearly identified | M | O, R | clearly identified | clearly identified | clearly identified | clearly identified |
| Kendall-Gallagher D et al. 2009 (19) | clearly identified | N | C, cross-sectional study of secondary analysis | clearly identified | clearly identified | not clearly identified | clearly identified |
| Van den Heede K et al. 2009 (33) | clearly identified | N | O, R | clearly identified | clearly identified | clearly identified | clearly identified |
| Seynaeve S et al. 2010 (24) | clearly identified | N | R, cross-sectional survey | clearly identified | clearly identified | not clearly identified | clearly identified |
| Blot SI et al. 2011 (16) | clearly identified | M | O, R | clearly identified | clearly identified | clearly identified | clearly identified |
| Daud-Galotti RM et al. 2012 (17) | clearly identified/not clearly identified | M | O, P | clearly identified | clearly identified | not clearly identified | clearly identified |
| Moneke N et al. 2013 (35) | clearly identified | N | C, survey CCNs | clearly identified | clearly identified | clearly identified | clearly identified |
| Thompson DA et al. 2013 (20) | clearly identified | N | RCT, Longitudinal | clearly identified | not clearly identified | not clearly identified | clearly identified |
| Valentin A et al. 2013 (23) | clearly identified | M | O, P, cross-sectional study | clearly identified | not clearly identified | not clearly identifies | clearly identified |
| Lucchini A et al. 2014 (28) | clearly identified | N | O, R | clearly identified | clearly identified | clearly identified | clearly identified |
| West E et al. 2014 (30) | clearly identified | N | O, R, cross-sectional study | clearly identified | clearly identified | not clearly identified | clearly identified |
| Lærkner E et al. 2016 (27) | clearly identified | N | RCT | clearly identified | clearly identified | clearly identified | clearly identified |
| Falk A-C et al. 2016 (25) | clearly identified | N | R, survey of registry data (patient) | clearly identified | clearly identified | clearly identified | clearly identified |
| Jansson M et al. 2020 (26) | clearly identified | N | O, R, cross-sectional study | clearly identified | clearly identified | not clearly identified | clearly identified |
The quality assessment (Table 2) revealed that 21 studies clearly identified the strengths and weaknesses of the research base and that 2 studies did not clearly identify research gaps or recommend further research. The implications for practice were not clearly identified in 10 of the 21 studies, but all studies had clearly identified ethics.
How is nursing competence in ICUs described?
The educational level of nurses working in ICUs is poorly described in studies in both nursing and multidisciplinary journals. Three studies described nurses’ competence level as formal education with a bachelor’s (33) or master’s degree (25,35). Two studies used the term “nurse” or “nurse in ICU” (24,26) without any description of the level of competence or education in critical care. Other studies used group terms such as “healthcare teams” (19), frontline staff (23), coronary care unit staff, or healthcare workers, both covering nurses and technicians (17).
Level of competence was also described in broad terms such as ICU nurses qualified to manage ventilators (16) or able to perform dialysis, mobilization, and weaning from mechanical ventilation (27). Some studies used more specialized terms such as “nurses with certification for the unit” (22), CCNs and intensive care nurses (ICN) (25,35), and ICU nurses (16,26,28) without describing the educational level. In one study, nurses were mentioned only as the product of a scoring system, without any further description of the level of competence (23).
The term skill or skill mix is used in several studies without the definitions of the skills involved (19,30,32). Only one study (30) distinguished between direct care and supernumerary nurses or those in administrative positions. Therefore, nurse competence was poorly described, educational level was often not mentioned, and several job titles were used, making it almost impossible to precisely interpret nursing competence.
How is nurse staffing in ICUs described, applied, and measured?
In the 21 studies (Table 1), we found different descriptions of nursing time consumption, such as RN hours per patient day (20,32) and nursing hours per patient day (33). Some studies used staffing numbers such as nurse-to-bed ratio (30), number of staff, and number of patients seen daily (23,30).
A fixed nurse-to-patient ratio was mentioned in six studies. The nurse-to-patient ratio was also included if a tool was used to assess nurse staffing in ICUs. The tools used were the Nine Equivalents of Nursing Manpower Use Score (NEMS) (23), the Nursing Care Recording System (NCR11) (27), the Therapeutic Intervention Scoring System (TISS-28) (24,29,36) or TIS (21), TISS-76 (26), ICNSS (26), and the Nursing Activities Score (NAS) (17,28). These tools measure the nursing requirements for individual patients and recommend the number of nurses in terms of nursing intensity and workload.
Some studies did not clearly state the number of nurses available, the number of nurses required, or the assessment tools used. Increased use of validated tools from 2012 was found in studies that assessed patients’ needs for care, rather than simply considering nurse-to-patient ratios (17,26–28,35).
How are nursing competence and staffing in ICUs associated with nurse-sensitive outcomes?
Nurse staffing correlated with nurses’ workload and infections as nurse-sensitive outcomes (Table 1) (16–23). Nurse staffing also correlated with ADEs or medication errors (19,23–24), unplanned extubation, or line removal (23,25). High nurse workload (i.e. caring for twice the usual number of patients) was related to the spread of nosocomial infections measured using TISS-28 in a 3-year prospective study from Slovenia (36). Kendall-Gallagher and Blegen analysed data from a large national data set of 15,846 patients from the United States and found that the incidence rate of catheter-associated urinary tract infections was associated with increased overtime and decreased if the proportion of certified nurses was higher (19). They also found a significantly lower incidence rate of central line-associated bloodstream infections if the ICU had more RN hours per patient day. The same result was found by Thompson et al. (20). If the ICU had more than 20 RN hours per patient day, it also had a lower incidence rate of central line-associated bloodstream infections. Kendall-Gallagher and Blegen (19) and Dancer et al. (21) examined the incidence of hygiene failures and found an association with understaffing, which means high nurse workload.
The incidence rate of ventilator-associated pneumonia in Europe decreased when the nurse-to-patient ratio was greater than 1:1 (16), although no significant differences were found after adjustment for confounders (i.e. knowledge and competence in ventilators). In Sweden, decreased time on ventilator was associated with a higher CCN-to-patient ratio, but the study did not report on any tools used to assess workload (25). A cohort study of patients with infections in an ICU in Switzerland found that low nurse staffing was associated with a risk of infections and that infections could be prevented by maintaining higher staffing levels (22). All nurses working in ICUs in this study were either trained or trainees in critical care. A later study found that excessive nursing workload, measured using NAS, was the main risk factor of healthcare-associated infections (17). In a study from Italy, Lucchini et al. found no link between NAS results and the risk of developing pressure ulcers (28).
The next nurse-sensitive outcomes of interest were ADEs or medication errors, which are considered determinants of patient safety and quality of care (19,23–24). In Belgium, ADEs were found to be associated with the mean severity of illness (Acute Physiology and Chronic Health Evaluation II [APACHE-II] and Sequential Organ Failure Assessment score [SOFA score] ) and nursing workload [TISS-28]. The incidence rate of ADEs was significantly higher on days when the nursing workload was high (24). Fewer hours of nursing care per patient day were related to a higher incidence rate of ADEs in a random sample of 48 ICUs in the United States (19). One study investigated the safety climate and found that frontline staff (i.e. nurses) who could prevent errors and who made safety a priority contributed to a reduction of medical errors (i.e. ADEs) (23).
At the patient level, dislodgement of tubes, lines, catheters, and drains was significantly related to workload assessed using NEMS (23). Unplanned extubation was more frequent (3–5.7%), with a lower nurse-to-patient ratio, especially in units not allowing physical hand restraints (25).
In research on safety climate, ICUs measure nurse-sensitive outcomes in terms of length of ICU stay (27) or mortality (20,26,29–34). In Denmark, a RCT by Laerkner et al. suggested that a 1:1 nurse-to-patient ratio and a no-sedation policy might result in lower costs related to shorter length of hospital stay (27). West et al. described survival rates and, after controlling for patient characteristics and workload, found that higher numbers of nurses per bed were associated with higher survival rates (30). Nursing hours per patient also affected the mortality rate in a study in Belgium (24). In Finland, Jansson et al. found that nursing workloads (TISS and ICNSS) were significantly higher in patients with multiple-organ failure and in non-survivors over a 10-year period (26). In Korea, additional patients per RN were associated with increased odds ratio for mortality (34). A lower mortality rate was reported with more nursing hours per patient (33). The leaders described the patterns of interaction to achieve patient outcomes (35) and especially with an increase number of infection (36).
Studies that used tools for workload were more likely to report significant patient outcome results (17, 23–27). The incidence rate of nosocomial infections increased when nurses’ workload (measured using NAS) was high and their level of competence was low (17). The incidence rate of ADEs increased with a higher workload (measured using TISS-28) or lower educational levels among nurses (24). The incidence rates of dislodgement of tubes, lines, catheters, and drains increased with higher workload (NEMS) and lower nurse-to-patient ratio (23,25). The length of hospital stay was shorter when patients were not sedated for ventilation, and this was also associated with a lower workload (NCR11) (27). Multiple-organ failure and mortality were associated with high workloads (TISS and ICNSS) (26).
Discussion
This scoping review focused on how the competence of nurses working in ICUs is described, applied, and associated with nurse-sensitive outcomes. Generally, the certification status of RNs has not been not described, making it impossible to link different levels of competence to outcomes. According to Kendall-Gallagher and Blegen (19), the relationship between the competence and certification of healthcare professionals and the safety of patients is a relatively new area of enquiry in nursing. However, specialty certification and the competence of RNs were related to patient safety (19). Measuring the relationship between the competencies of individual RNs and outcomes is also methodologically difficult because nurse is used as a general expression or nurses are considered part of multi-disciplinary teams, characterized as a group such as frontline staff (23), without any more specific information.
The existing standards for nurse-to-patient ratios or nurse staffing are predominantly opinion based rather than supported by research (11). Further descriptions of the different types of nursing certification and the work of nurses in the ICU, such as performing dialysis, mobilisation, and weaning from ventilation, are needed to link competence to patient outcomes. No international standardisation has been established across the various certifications, and no study to date has compared the effects of different certifications in ICUs. Researchers should be encouraged to provide better descriptions of the context, educational level, team skill mix (e.g. pharmacists, physiotherapists, and assistants), activities, turnover, educational programme for new employees, and nurse-to-patient ratio to enable readers to evaluate the transferability of studies.
We found that nosocomial infections (17, 19–22,25) and ADEs (19,23–24) were related to higher workloads or lower nurse ratios. Several studies have concluded that a safety climate apparently contributes to the reduction of negative results among frontline staff (i.e. nurses), although all acknowledged that nurses remain vulnerable to human error (23). Length of hospital stay is a major concern for workload and costs, but evidence of any connection to workload is lacking. Sakr et al. found that a nurse-to-patient ratio of 1:1.5 or higher was the only significant factor of reduced mortality rate (37). In Norway, laws and regulations on staffing needs and quality of care also regulate leadership and organisational factors. Healthcare professionals, including nurses, should have enough up-to-date training and knowledge on how to care for patients and relatives (38).
Several studies (20,26,29–33) have provided evidence of associations and correlations between staffing levels and mortality. This was confirmed by data from 65 ICUs, which indicated that a higher number of nurses per ICU bed, especially for high-dependency patients, was associated with better survival or reduced mortality (39). In a study of CCNs in the United States, Rothschild et al. estimated different staffing models of nurse-to-patient ratio and found that better staffing could improve patient outcomes and provide financial savings associated with adverse event prevention (40). A multi-centre study from the United States reported that low nurse staffing in ICUs increased the mortality rate, the number of healthcare-associated infections, and “failure to rescue” (41). The number of nurses had the greatest impact on patients’ mortality risk (41). The nurse staffing levels in ICUs are crucial, particularly for patient surveillance and the reduction of mortality rates (1). This was consistent with the findings of studies of the general acute care population and nurse staffing (41).
Communication within the professional team and a safety environment are important organisational factors (1). The professional team in the ICU normally includes physicians, pharmacists, physiotherapists, social workers, nutritionists, and nurses (1). When professional teams had standard meetings that included nurses and settled daily individual plans for care, the mortality rate and length of ICU stay were reduced (42–45). This was supported by the results from Checkley et al., who found that the adjusted annual ICU mortality rate was 5.8% lower among ICUs with daily care reviews (39). Dietz et al. found that teamwork could improve the safety environment in terms of reduced injuries and adverse events, lower risks of complications, and improved clinical outcomes (46). They also highlighted the importance of nurse competence and specialisation for both continuity and complexity of care. Nurse staffing is essential and has an impact on organisational factors for improving the quality of care.
The methodological quality appraisal (Table 2) of the included studies showed all a high quality according to the CASP criteria. However, suggestions for implications for practice were missing in 50% of the studies.
Limitations and strengths
A potential limitation of this study is that we only searched for studies published in English and Scandinavian. It is possible that relevant studies were published in other languages. A weakness of our review was that two studies (22,30) had results from the data collection based on the same patients from one ICU in Switzerland. A scoping review has inherent limitations because the focus is to provide breadth rather than depth of information on a particular topic (13,15). As such, a quality appraisal is generally not conducted in a scoping review. However, this method was appropriate given that our objective was to map out the evidence on how levels of nursing competence and staffing in ICUs were described and associated with nurse-sensitive outcomes in the literature. A strength of this study was the widespread inclusion of journals and the inclusion of both small and large studies in several countries (13). Further studies should investigate CCNs and how their competence in direct care affects nurse-sensitive outcomes in ICUs.
Conclusion
We found associations between education, nurse staffing, and nurse-sensitive outcomes in intensive and critical care units. To highlight the association between advanced nursing competence in critical care and research, the level of competence of CCNs must be better described. This review reveals a need for more research on the effect of advanced nursing competence in ICUs. Patients’ need for advanced nursing competence must be assessed using validated tools. It is important to ensure that CCNs have the competence to undertake research to evaluate and continuously improve the treatment and care of patients in ICUs.
Contributions
SKS and BS searched and screened for studies in databases and used checklists for quality control (CASP). SKS and JB performed a review of the literature according to the PRISMA checklist. EG, SKS, and BS drafted the manuscript. SKS, SF, BSH, JB, and EG were active in the writing process and approved the final version.
Funding source
This research was funded by the Norwegian Nurses Organisation Professional Interest Group of Intensive Care Nurses and the first author’s hospital and university workplace.
Ethics statement
Ethics approval was not required for the scoping review of the literature.
Conflict of interest
The authors have no past or present affiliation with any parties who would have an interest in the outcome of this review, which could constitute a conflict of interest.
Relevance to clinical practice
- Advanced nursing competence in ICUs must be better described in research and linked to nurse-sensitive outcomes.
- A validated tool to assess patients’ need for care and nurses’ workload is necessary to measure the quality of nurse-sensitive outcomes in critical care.
- It is important to enable critical care nurses (through post-graduate qualifications or a master’s degree) to undertake research to show and continuously improve their impact on the treatment and care of patients.
References
- 1. Greaves J, Goodall D, Berry A, Shrestha S, Richardson A, et al. Nursing workloads and activity in critical care: a review of the evidence. Intens Crit Care Nur. 2018;48:10–20. https://doi.org/10.1016/j.iccn.2018.06.002
- 2. Endacott R, Jones C, Bloomer MJ, Boulanger C, Ben Nun M, et al. The state of critical care nursing education in Europe: an international survey. Intens Care Med. 2015;41(12):2237. https://doi.org/10.1007/s00134-015-4072-y
- 3. Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, et al. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. 2014;383:1824–30. https://doi.org/10.1016/S0140-6736(13)62631-8
- 4. Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, et al. Patient safety, satisfaction, and quality of hospital care: cross-sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012;344:e1717. https://doi.org/10.1136/bmj.e1717
- 5. Fukada M. Nursing competency: definition, structure and development. Yonago Acta Med. 2018;61:001–7.
- 6. Penoyer DA. Nurse staffing and patient outcomes in critical care: a concise review. Crit Care Med. 2010;38(7):1521–8. https://doi.org/10.1097/CCM.0b013e3181e47888
- 7. Bakon S, Christensen M, Barker-Gregory N. Appropriate staffing in critical units: a review of the literature. Singap Nurs J. 2016;43(3):16–24.
- 8. Lakanmaa RL, Suominen T, Perttilä J, Ritmala-Castrèn M, Vahlberg T, et al. Graduating nursing students’ basic competence in intensive and critical care nursing. J Clin Nurs. 2014;23(5–6):645–53. https://doi.org/10.1111/jocn.12244
- 9. Doran DM, Harrison MB, Laschinger HS, Hirdes JP, Rukholm E, et al. Nursing-sensitive outcomes data collection in acute care and long-term-care settings. Nurs Res. 2006;55(2):S75–81. https://doi.org/10.1097/00006199-200603001-00012
- 10. Heslop L, Lu S. Nursing-sensitive indicators: a concept analysis. J Adv Nurs. 2014;70(11):2469–82. https://doi.org/10.1111/jan.12503
- 11. Gill FJ, Leslie GD, Grech C, Latour JM. A review of critical care nursing staffing, education and practice standards. Aust Crit Care. 2012;25(4):224–37. https://doi.org/10.1016/j.aucc.2011.12.056
- 12. Norsk Sykepleierforbund. Bemanningsstandard for intensivsykepleie NSFLIS 2015 [English translation] [Internet]. Oslo: Norsk Sykepleierforbund; August 2015 [cited July 31, 2023]. Available from: https://www.nsf.no/sites/default/files/inline-images/rsyGhR3uL7SwEdYapOfY8eqX2azywFKv8Kgf0hg19vbfr4lc15.pdf
- 13. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method. 2005;8(1):19–32. https://doi.org/10.1080/1364557032000119616
- 14. Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, et al. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–85. https://doi.org/10.1002/jrsm.1123
- 15. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2): 91–108. https://doi.org/10.1111/j.1471-1842.2009.00848.x
- 16. Blot SI, Serra ML, Koulenti D, Lisboa T, Deja M, et al. Patient to nurse ratio and risk of ventilator-associated pneumonia in critically ill patients. Am J Crit Care. 2011;20(1):E1. https://doi.org/10.4037/ajcc2011555
- 17. Daud-Gallotti R, Costa S, Guimarães T, Inoue E, Figueiredo W, et al. Nursing workload as a risk factor for healthcare associated infections in ICU: a prospective study. PLOS One. 2012;7(12):e52342. https://doi.org/10.1371/journal.pone.0052342
- 18. Hugonnet S, Uçkay I, Pittet D. Staffing level: a determinant of late-onset ventilator-associated pneumonia. Crit Care. 2007;11(4):R80. https://doi.org/10.1186/cc5974
- 19. Kendall-Gallagher AD, Blegen AM. Competence and certification of registered nurses and safety of patients in intensive care units. J Nurs Admin. 2010;40(10 Suppl):S68–77. https://doi.org/10.1097/NNA.0b013e3181f37edb
- 20. Thompson D, Hsu Y, Chang B, Marsteller J. Impact of nursing staffing on patient outcomes in intensive care unit. J Nurs Care. 2013;2:2. https://doi.org/10.4172/2167-1168.1000128
- 21. Dancer SJ, Coyne M, Speekenbrink A, Samavedam S, Kennedy J, et al. MRSA acquisition in an intensive care unit. Am J Infect Control. 2006;34(1):10–7. https://doi.org/10.1016/j.ajic.2005.08.009
- 22. Hugonnet S, Chevrolet J-C, Pittet D. The effect of workload on infection risk in critically ill patients. Crit Care Med. 2007;35(1):76–81. https://doi.org/10.1097/01.CCM.0000251125.08629.3F
- 23. Valentin A, Schiffinger M, Steyrer J, Huber C, Strunk G. Safety climate reduces medication and dislodgement errors in routine intensive care practice. Intens Care Med. 2013;39(3):391–8. https://doi.org/10.1007/s00134-012-2764-0
- 24. Seynaeve S, Reyntiens D, Vandenplas D, Verbrugghe W, Claes B, et al. Adverse drug events in the critical care unit. Crit Care. 2010;14(1):P448. https://doi.org/10.1186/cc8680
- 25. Falk AC, Wallin EM. Quality of patient care in the critical care unit in relation to nurse patient ratio: a descriptive study. Intens Crit Care Nurs. 2016;35:74–9. https://doi.org/10.1016/j.iccn.2016.01.002
- 26. Jansson M, Ohtonen P, Syrjälä H, Ala-Kokko T. The proportion of understaffing and increased nursing workload are associated with multiple organ failure: a cross-sectional study. J Adv Nurs. 2020;76(8):2113–24. https://doi.org/10.1111/jan.14410
- 27. Laerkner E, Stroem T, Toft P. No-sedation during mechanical ventilation: impact on patients’ consciousness, nursing workload and costs. Nurs Crit Care. 2016;21(1):28–35. https://doi.org/10.1111/nicc.12161
- 28. Lucchini A, De Felippis C, Elli S, Schifano L, Rolla F, et al. Nursing Activities Score (NAS): 5 years of experience in the intensive care units of an Italian university hospital. Intens Crit Care Nurs. 2014;30(3):152–8. https://doi.org/10.1016/j.iccn.2013.10.004
- 29. Kiekkas P, Sakellaropoulos GC, Brokalaki H, Manolis E, Samios A, et al. Association between nursing workload and mortality of intensive care unit patients. J Nurs Scholarsh. 2008;40(4):385–90. https://doi.org/10.1111/j.1547-5069.2008.00254.x
- 30. West E, Barron DN, Harrison D, Rafferty AM, Rowan K, et al. Nurse staffing, medical staffing and mortality in intensive care: an observational study. Int J Nurs Stud. 2014;51(5):781–94. https://doi.org/10.1016/j.ijnurstu.2014.02.007
- 31. Tourangeau AE, Doran DM, Hall LM, O’Brien Pallas L, Pringle D, et al. Impact of hospital nursing care on 30-day mortality for acute medical patients. J Adv Nurs. 2007;57(1):32–44. https://doi.org/10.1111/j.1365-2648.2006.04084.x
- 32. Sales A, Sharp N, Li Y-F, Lowy E, Greiner G, et al. The association between nursing factors and patient mortality in the veterans health administration: the view from the nursing unit level. Med Care. 2008;46(9):938–45. https://doi.org/10.1097/MLR.0b013e3181791a0a
- 33. Van Den Heede K, Lesaffre E, Diya L, Vleugels A, Clarke SP, et al. The relationship between inpatient cardiac surgery mortality and nurse numbers and educational level: analysis of administrative data. Int J Nurs Stud. 2009;46(6):796–803. https://doi.org/10.1016/j.ijnurstu.2008.12.018
- 34. Cho S-H, Yun S-C. Bed-to-nurse ratios, provision of basic nursing care, and in-hospital and 30-day mortality among acute stroke patients admitted to an intensive care unit: cross-sectional analysis of survey and administrative data. Int J Nurs Stud. 2009;46(8):1092–101. https://doi.org/10.1016/j.ijnurstu.2009.02.001
- 35. Moneke JN, Umeh JO. Factors influencing critical care nurses’ perception of their overall job satisfaction: an empirical study. J Nurs Admin. 2013;43(4):201–7. https://doi.org/10.1097/NNA.0b013e31828958af
- 36. Blatnik J, Lešničar G. Propagation of methicillin-resistant Staphylococcus aureus due to the overloading of medical nurses in intensive care units. J Hosp Infect. 2006;63(2):162–6. https://doi.org/10.1016/j.jhin.2005.11.013
- 37. Sakr Y, Moreira CL, Rhodes A, Ferguson ND, Kleinpell R, et al. The impact of hospital and ICU organizational factors on outcome in critically ill patients: results from the extended prevalence of infection in intensive care study. Crit Care Med. 2015;43(3):519–26. https://doi.org/10.1097/CCM.0000000000000754
- 38. Health Personnel Act. LOV-1999-07-02-64 [cited February 1, 2023]. Available from: https://lovdata.no/lov/1999-07-02-64
- 39. Checkley W, Martin G, Brown SM, Chang S, Dabbagh O, et al. Structure, process, and annual ICU mortality across 69 centers: United States Critical Illness and Injury Trials Group Critical Illness Outcomes Study. Crit Care Med. 2014;42(2):344–56. https://doi.org/10.1097/CCM.0b013e3182a275d7
- 40. Rothschild JM, Bates DW, Franz C, Soukup JR, Kaushal R. The costs and savings associated with prevention of adverse events by critical care nurses. J Crit Care. 2009;24(3):471.e1–7. https://doi.org/10.1016/j.jcrc.2007.12.021
- 41. Aiken L, Rafferty AM, Sermeus W. Caring nurses hit by a quality storm. Nurs Stand. 2014;28(35):22–5. https://doi.org/10.7748/ns2014.04.28.35.22.s26
- 42. Alameddine M, Dainty KN, Deber R, Sibbald WJB. The intensive care unit work environment: current challenges and recommendations for the future. J Crit Care. 2009;24(2):243–8. https://doi.org/10.1097/CCM.0b013e3181e47888
- 43. Carayon P, Gürses AP. A human factors engineering conceptual framework of nursing workload and patient safety in intensive care units. Intens Crit Care Nurs. 2005;21(5):284–301. https://doi.org/10.1016/j.iccn.2004.12.003
- 44. Hansen B, Severinsson E. Dissemination of research-based knowledge in an intensive care unit – a qualitative study. Intens Crit Care Nurs. 2009;25(3):147–54. https://doi.org/1016/j.iccn.2009.02.005
- 45. Pronovost P, Wu AW, Dorman T, Morlock L. Building safety into ICU care. J Crit Care. 2002;17(2):78–85. https://doi.org/10.1053/jcrc.2002.34363
- 46. Dietz AS, Pronovost PJ, Mendez-Tellez PA, Wyskiel R, Marsteller JA, et al. A systematic review of teamwork in the intensive care unit: what do we know about teamwork, team tasks, and improvement strategies? J Crit Care. 2014;29(6):908–14. https://doi.org/10.1016/j.jcrc.2014.05.025

Search ID# |
Search Terms |
|---|---|
| S40 | S37 AND S38 |
| S39 | S37 AND S38 |
| S38 | S30 OR S31 OR S32 OR S33 OR S34 |
| S37 | S29 AND S36 |
| S36 | S28 OR S35 |
| S35 | (MH “Acute Care”) |
| S34 | (MH “Infection Control+”) |
| S33 | (MH “Length of Stay”) |
| S32 | (MH “Treatment Errors+”) |
| S31 | (MH “Adverse Health Care Event+”) OR “adverse events” |
| S30 | (MH “Skill Mix+”) |
| S29 | (MH “Personnel Staffing and Scheduling+”) OR “staffing” |
| S28 | (MH “Critical Care Nursing+”) |
| S27 | S13 OR S22 |
| S26 | S6 AND S10 |
| S25 | S6 AND S10 AND S12 |
| S24 | S6 AND S9 |
| S23 | S1 AND S6 |
| S22 | S6 AND S12 |
| S21 | S4 AND S6 AND S12 |
| S20 | S6 AND S19 |
| S19 | S7 AND S12 |
| S18 | S1 AND S4 |
| S17 | S1 AND S5 |
| S16 | S1 AND S2 |
| S15 | S1 AND S14 |
| S14 | S3 AND S12 |
| S13 | S1 AND S12 |
| S12 | S2 OR S11 |
| S11 | (MH “Acute Care”) |
| S10 | (MH “Infection Control+”) |
| S9 | (MH “Time Management”) |
| S8 | (MH “Appointment and Scheduling Information Systems”) |
| S7 | (MH “Personnel Management+”) |
| S6 | (MH “Clinical Competence+”) |
| S5 | (MH “Nursing Care+”) |
| S4 | (MH “Risk Management+”) |
| S3 | (MH “Treatment Errors”) OR (MH “Health Care Errors”) |
| S2 | (MH “Critical Care”) OR “intensive care” |
| S1 | (MH “Personnel Staffing and Scheduling+”) |